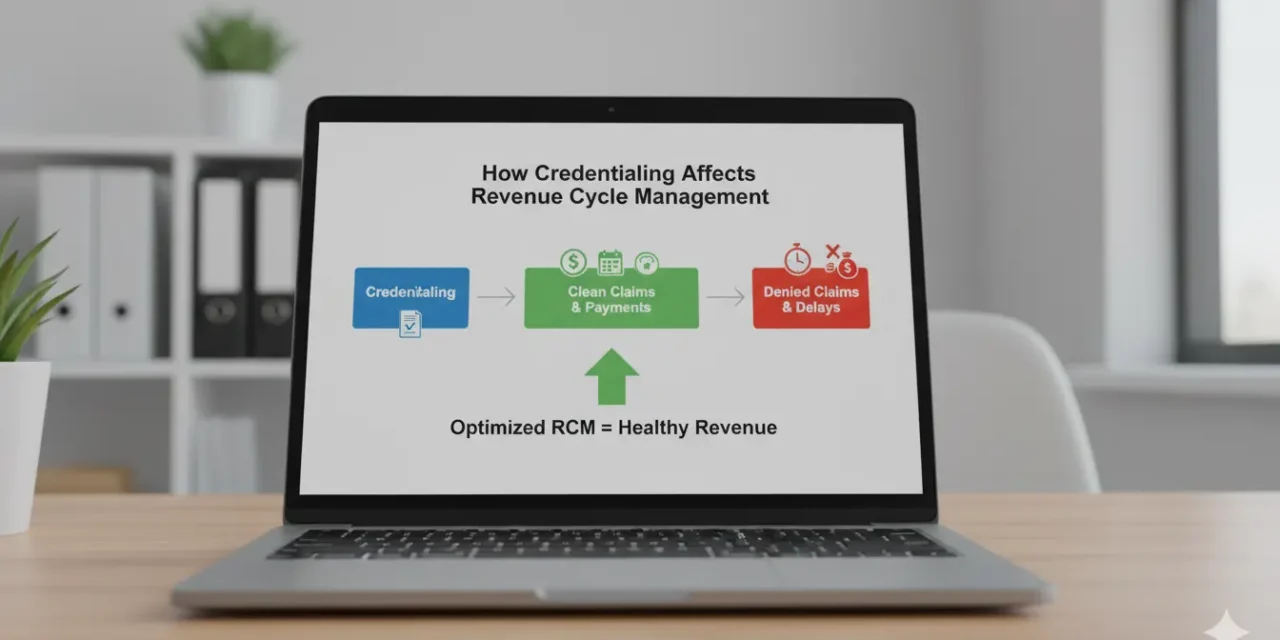
Credentialing and revenue cycle management (RCM) connect directly—without approved provider credentials, claims don’t get paid, stalling your practice’s cash flow from day one. Hospitals, payers, and networks require up-to-date enrollment before reimbursing services, so delays in credentialing mean delayed or rejected payments that ripple through your entire billing process. Think of credentialing as the front...
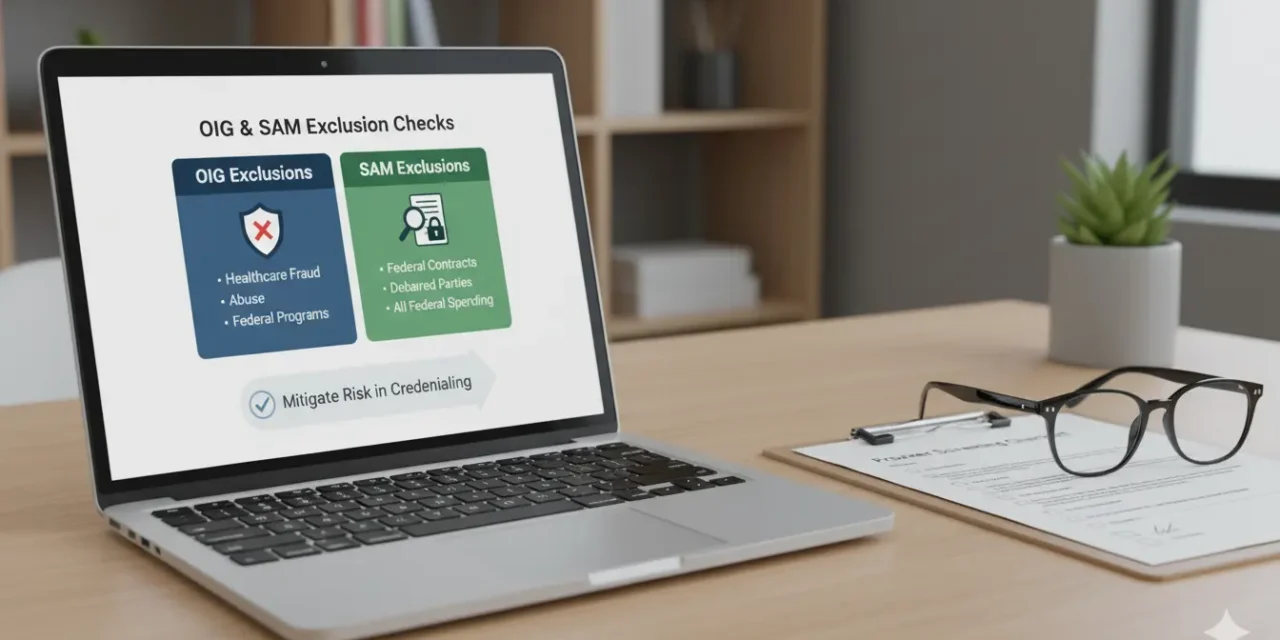
OIG and SAM exclusion checks stand as essential safeguards in the credentialing process. They verify that no providers, staff, or vendors on your team appear on federal exclusion lists, ensuring full compliance before granting privileges or billing privileges. Skipping these checks exposes your practice to major financial and legal threats. Federal rules demand clean records...
Background checks form a core part of the credentialing process, helping healthcare organizations confirm a provider’s qualifications and history before granting privileges. They verify education, licenses, and any past issues to ensure only trusted professionals deliver care. These checks protect patients by spotting risks like sanctions or malpractice patterns early, while reducing legal and financial...
Healthcare organizations rely on the National Practitioner Data Bank (NPDB) to guide credentialing and privileging decisions. Credentialing verifies a provider’s qualifications, training, and track record, while privileging defines the exact services they can deliver at a facility. This system protects patients by ensuring only vetted professionals provide care. The NPDB acts as a trusted clearinghouse...
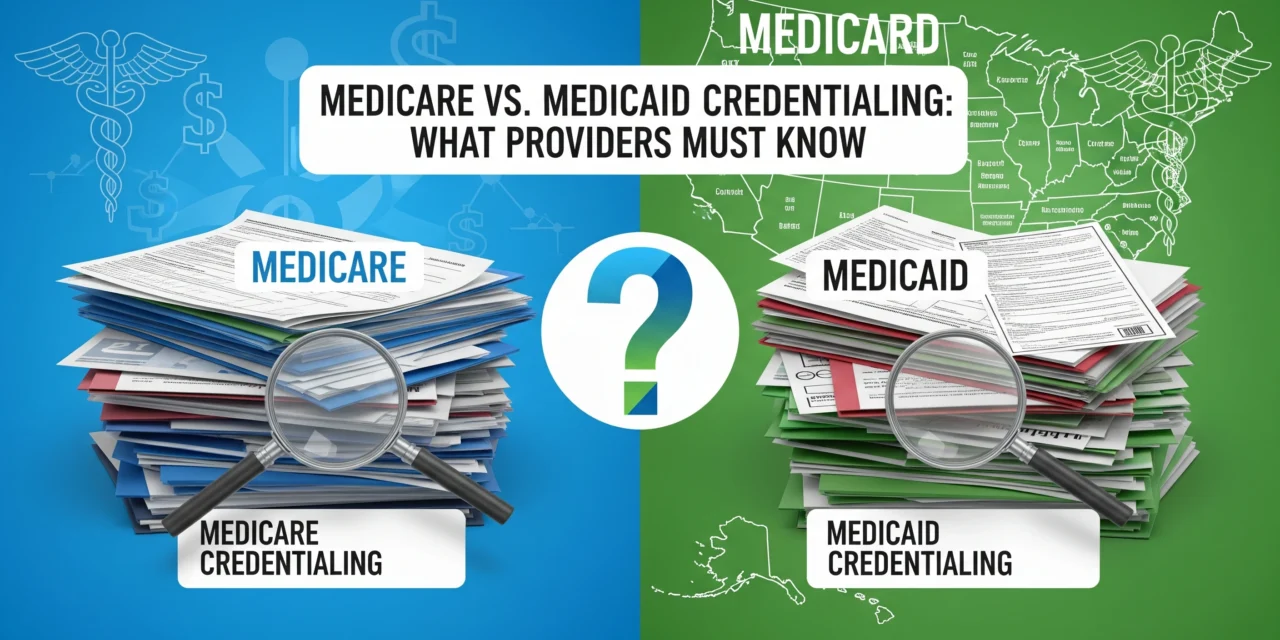
Medicare and Medicaid are two major government health insurance programs, but their credentialing processes differ significantly for providers. Medicare is a federal program for seniors and certain disabled individuals, managed uniformly by the Centers for Medicare & Medicaid Services (CMS). Medicaid is jointly funded by the federal and state governments, so each state runs its...
Blue Cross Blue Shield (BCBS) is one of the largest health insurance networks in the U.S., covering millions of patients across regional plans nationwide. If you want to treat BCBS patients and get reimbursed, credentialing is a must—it’s how BCBS verifies your qualifications before approving you for their network. Without credentialing, you can’t bill...
UnitedHealthcare (UHC) credentialing is the process by which UHC reviews your professional qualifications—like your licenses, education, and background—to make sure you meet their standards before you can join their provider network. Providers must complete credentialing before billing UHC for services. Without it, claims will be denied, and you can’t see UHC patients or get reimbursed....
Credentialing is a process where insurance companies like Aetna check your background to make sure you’re qualified to provide healthcare services. It’s like Aetna’s way of ensuring you have the right education, licenses, and experience to safely care for their members. Aetna requires credentialing before they accepts claims from providers. This step helps protect patients...
The Provider Enrollment, Chain, and Ownership System (PECOS) is Medicare’s official online platform designed to help healthcare providers, groups, and suppliers manage their Medicare enrollment smoothly. Instead of dealing with complicated paper forms, PECOS offers a digital way to apply, update, and maintain your Medicare enrollment information all in one place. Managed by the Centers...
Recredentialing is one of the most important — but often overlooked — parts of staying active with insurance networks. Even if a provider has been credentialed before, payers require regular rechecks to ensure they still meet all quality, licensure, and compliance standards. Whether you’re a solo provider, part of a group practice, or manage a...