Credentialing has always been one of the biggest roadblocks for healthcare organizations. Whether you run a growing mental health group, a primary care clinic, a specialty practice, or an MSO, you already know the problem — every new provider means more paperwork, more follow-ups with payers, and long waiting periods before they can start seeing...
CAQH ProView is an online system where healthcare providers keep all their professional information in one place. Think of it as your digital credentialing profile that insurance companies rely on. Instead of sending your licenses, education details, and work history to every payer separately, you upload everything once into CAQH ProView—and payers pull the information...
If you’re a mental health provider, whether you’re a therapist, counselor, psychologist, or social worker, credentialing is one of those tasks you can’t avoid. Insurance companies want to verify your education, license, training, and background before they let you join their network. And without being in-network, it’s harder to get steady patients, and even harder...
Getting credentialed with an insurance company like Cigna is one of the most important steps for any healthcare provider looking to grow their practice. It’s what allows you to join Cigna’s provider network, see patients covered by their plans, and get paid for your services without billing headaches. In simple terms, credentialing is the process...
If you’re a Nurse Practitioner (NP) or about to become one, you’ve probably heard the word credentialing more than once. But what exactly does it mean — and why should you care? In the simplest terms, credentialing is the process that confirms you’re licensed, certified, and qualified to provide care and bill payers (like Medicare,...
Credentialing is the process that proves you’re licensed, qualified, and ready to work as a therapist or mental health professional. It isn’t just a paperwork hurdle—credentialing is what lets you join insurance networks, earn reimbursement for your services, and build trust with both clients and payers. Without it, you risk missing out on clients who rely...
If you’re a new provider ready to launch your practice, there’s one key hurdle you can’t skip: getting credentialed. Credentialing is what lets you join insurer networks, bill for services, and actually start seeing patients—they don’t just hand you that approval overnight. When it takes too long, your billing is stalled, and your revenue drops....
Let’s talk about credentialing in healthcare—a process that basically means double-checking that a provider’s education, licenses, training, and all the necessary permissions (like payer enrollment and facility privileges) are up to standard. It’s the background check step that proves a doctor or provider is legit and allowed to treat patients and get paid by insurers....
When people talk about credentialing, it might sound like a dry administrative task. But in healthcare (and other regulated industries), credentialing is absolutely critical. It’s your system’s gatekeeper: verifying that a provider or professional is truly qualified, licensed, and safe for patients or clients. Mess it up, and the consequences are real — from lost...
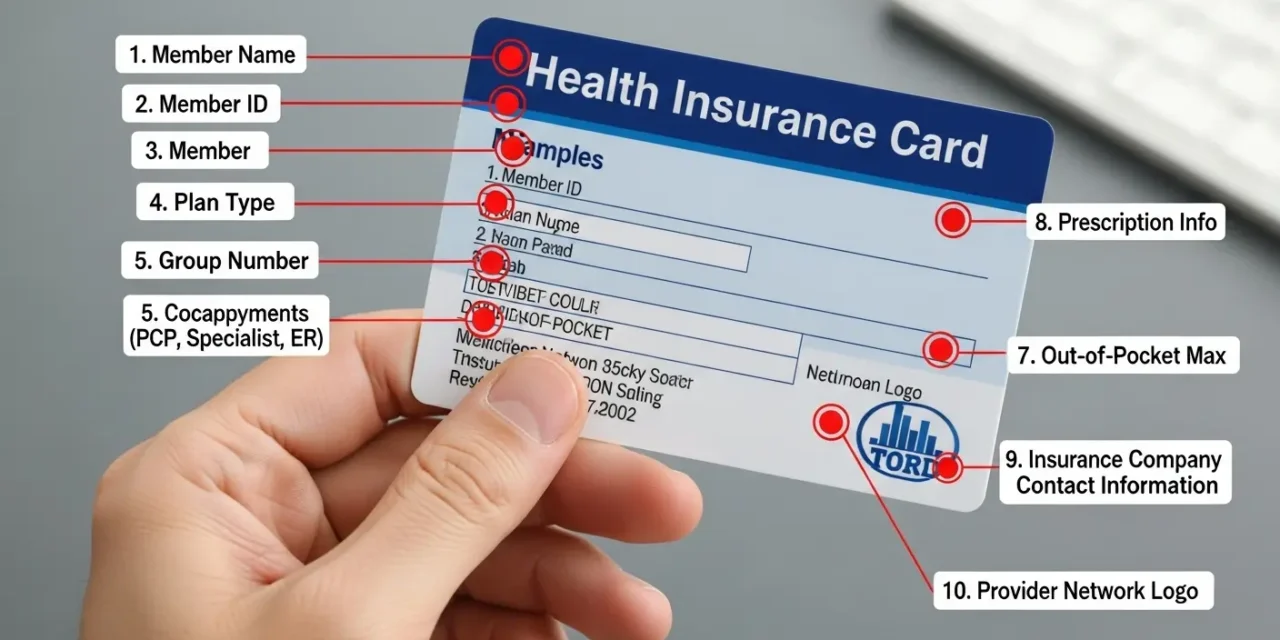
For healthcare providers, a patient’s health insurance card is more than just identification. It is the key to accurate billing, swift claims processing, and ensuring seamless patient care. Every insurance card contains important information about coverage, payers, plan types, and patient eligibility, but the layout and details can vary widely from one insurer to another. Misreading...